Osteoporosis
Osteoporosis is often called the “silent disease,” yet its impact on global health is anything but quiet. This condition weakens bones, making them fragile and prone to fractures—even from minor falls or everyday movements. Affecting millions worldwide, osteoporosis is a leading cause of disability among older adults and carries significant economic and social consequences. Despite its prevalence, many people remain unaware of its risk factors, prevention strategies, and long-term effects. In this article, we’ll explore 25 fascinating facts about osteoporosis, covering everything from its biological mechanisms and diagnostic standards to lifestyle prevention and global awareness campaigns. Whether you’re a healthcare professional, a fitness enthusiast, or simply curious about bone health, these insights will help you understand why osteoporosis deserves attention and how proactive measures can make a difference.
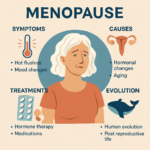
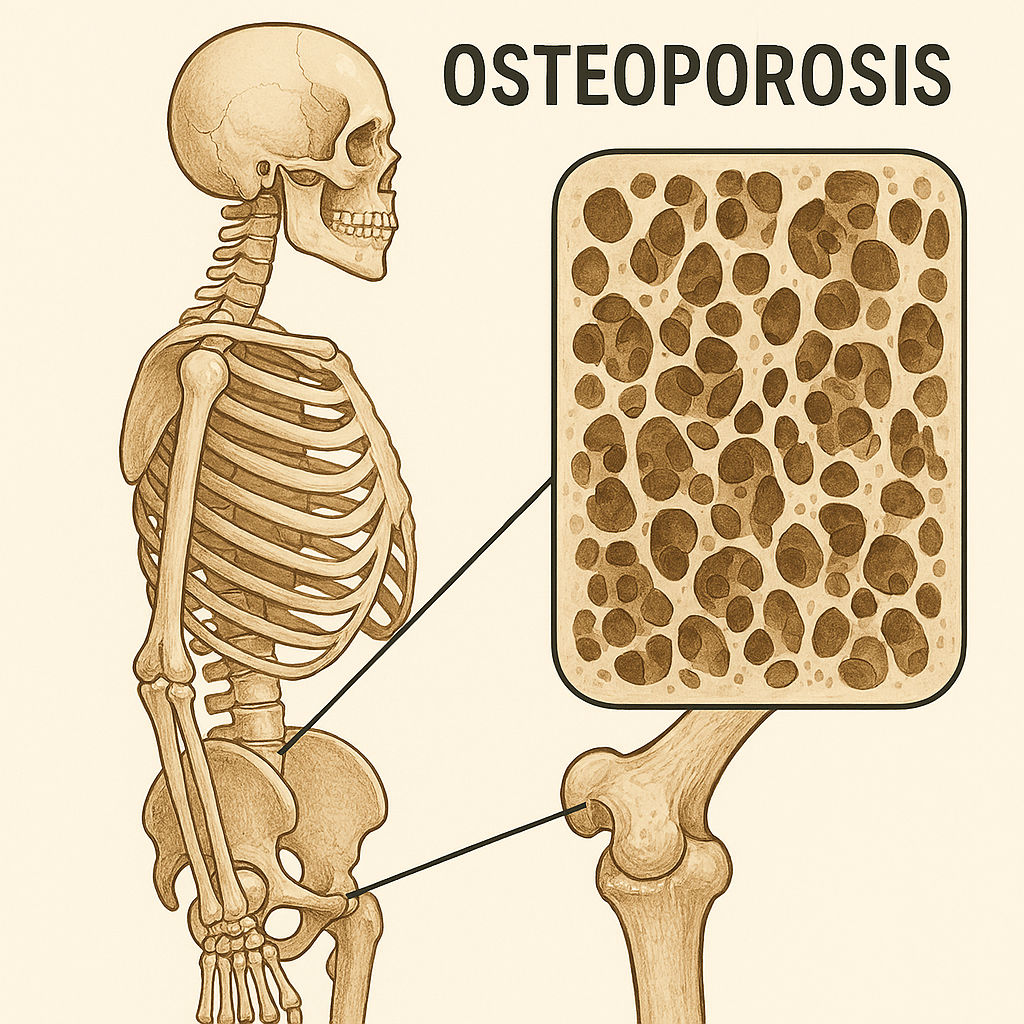
1. Definition of Osteoporosis
Osteoporosis is a chronic skeletal disorder characterized by a reduction in bone mass and deterioration of bone microarchitecture, leading to fragile bones that are highly susceptible to fractures. Unlike normal bone, which has a dense and strong structure, osteoporotic bone becomes porous and brittle due to an imbalance between bone formation and resorption. This condition is systemic, meaning it affects the entire skeleton rather than isolated areas. The term “osteoporosis” literally translates to “porous bone,” reflecting the microscopic holes that develop within bone tissue. These structural changes compromise bone strength, making even minor falls or stresses potentially catastrophic. Osteoporosis is not merely a natural consequence of aging—it is a pathological process influenced by hormonal changes, nutritional deficiencies, and lifestyle factors. Understanding this definition is crucial because it underscores the importance of early detection and preventive strategies to maintain skeletal integrity throughout life.
2. Silent Disease
Osteoporosis is often referred to as the “silent disease” because it progresses without obvious symptoms until a fracture occurs. Unlike conditions that present with pain or visible signs early on, osteoporosis can remain undetected for years while bones gradually weaken. This stealthy nature makes it particularly dangerous, as individuals may not realize they are at risk until they suffer a debilitating fracture, often in the hip, spine, or wrist. These fractures can lead to chronic pain, loss of mobility, and even increased mortality. The silent progression emphasizes the need for proactive screening, especially for older adults and those with risk factors. Public health campaigns often stress this point to encourage bone density testing before irreversible damage occurs.
3. Most Common Cause of Fractures in Elderly
Among older adults, osteoporosis is the leading cause of fractures, particularly in weight-bearing bones like the hip and spine. These fractures are not only painful but also life-altering, often resulting in hospitalization, surgery, and long-term rehabilitation. Hip fractures, for example, frequently lead to loss of independence and increased mortality rates within a year of the injury. Vertebral fractures can cause chronic back pain and spinal deformities, such as kyphosis, which further impair mobility and quality of life. Wrist fractures, while less severe, can still limit daily activities. The prevalence of these fractures underscores the importance of preventive measures, including fall-proofing homes and maintaining bone health through diet and exercise.
4. Prevalence
Osteoporosis affects millions worldwide, with prevalence increasing dramatically with age. Approximately 15% of individuals over 50 and up to 70% of those over 80 have osteoporosis, making it one of the most common age-related conditions. This widespread occurrence places a significant burden on healthcare systems, particularly in aging populations. The high prevalence also means that osteoporosis is not a niche concern—it is a major public health issue requiring coordinated efforts in screening, education, and treatment. Understanding these statistics helps contextualize why osteoporosis research and prevention programs receive substantial attention globally.
5. Gender Differences
Women are disproportionately affected by osteoporosis, primarily due to hormonal changes after menopause. Estrogen plays a critical role in maintaining bone density, and its decline during menopause accelerates bone loss. Men are not immune, however; they experience gradual testosterone decline, which also impacts bone health. While men typically develop osteoporosis later in life, their fractures tend to be more severe due to larger body mass and delayed diagnosis. Gender differences in osteoporosis prevalence highlight the need for tailored prevention strategies, such as hormone replacement therapy for women and early screening for men with risk factors.
6. Bone Density Peak
Bone density reaches its maximum strength during early adulthood, typically in the late 20s to early 30s. This peak bone mass serves as a critical determinant of future bone health because it represents the highest level of mineralization and structural integrity the skeleton will achieve. After this point, bone remodeling continues throughout life, but the balance shifts—bone resorption begins to outpace bone formation. This gradual decline accelerates with age and hormonal changes, particularly after menopause in women. Achieving optimal peak bone mass through proper nutrition, physical activity, and lifestyle choices during youth is essential because it provides a buffer against age-related bone loss. Individuals who fail to reach adequate peak bone density are at significantly higher risk of developing osteoporosis later in life.
7. Hormonal Influence
Hormones play a pivotal role in maintaining bone health, and their decline is a major factor in osteoporosis development. Estrogen, in particular, is crucial for regulating bone remodeling by inhibiting osteoclast activity, which breaks down bone tissue. When estrogen levels drop sharply during menopause, bone resorption accelerates, leading to rapid bone loss in women. Similarly, testosterone in men supports bone density, and its gradual decline with age contributes to osteoporosis risk, albeit at a slower rate than in women. Hormonal imbalances caused by medical conditions or treatments, such as surgical removal of ovaries or long-term corticosteroid use, can also trigger early-onset osteoporosis. Understanding this hormonal connection underscores why hormone replacement therapy and other endocrine interventions are often considered in osteoporosis management.
8. Risk Factors
Osteoporosis is influenced by a combination of modifiable and non-modifiable risk factors. Non-modifiable factors include age, gender, and genetics—women and older adults are inherently more vulnerable. Modifiable factors encompass lifestyle choices such as smoking, excessive alcohol consumption, and physical inactivity, all of which accelerate bone loss. Nutritional deficiencies, particularly in calcium and vitamin D, further compromise bone strength. Certain medications, including corticosteroids and chemotherapy drugs, can also weaken bones over time. Recognizing these risk factors is essential for prevention, as many can be addressed through lifestyle changes and medical interventions. Public health campaigns often emphasize these points to encourage proactive bone health management.
9. Secondary Causes
While primary osteoporosis is linked to aging and hormonal changes, secondary osteoporosis arises from other medical conditions or treatments. Diseases such as hyperthyroidism, chronic kidney disease, and gastrointestinal disorders that impair nutrient absorption can significantly impact bone health. Eating disorders like anorexia nervosa also contribute to bone loss due to inadequate nutrition and hormonal disruptions. Surgical procedures, such as oophorectomy (removal of ovaries), can precipitate early menopause and accelerate bone deterioration. Additionally, prolonged use of certain medications, including anticonvulsants and glucocorticoids, is a well-documented cause of secondary osteoporosis. Identifying these underlying conditions is critical for effective treatment, as addressing the root cause often improves bone health outcomes.
10. Diagnostic Standard
The gold standard for diagnosing osteoporosis is the DEXA scan (Dual-energy X-ray absorptiometry), which measures bone mineral density (BMD) with high precision. Results are expressed as a T-score, comparing an individual’s bone density to that of a healthy young adult. A T-score of −2.5 or lower confirms osteoporosis, while scores between −1.0 and −2.4 indicate osteopenia, a precursor to osteoporosis. This diagnostic tool is non-invasive, quick, and widely available, making it the cornerstone of osteoporosis screening programs. Regular bone density testing is recommended for women over 65 and men over 70, or earlier for individuals with risk factors such as previous fractures or long-term steroid use. Early detection through DEXA scans enables timely intervention, reducing the risk of debilitating fractures.
11. Bone Remodeling Imbalance
Bone health depends on a delicate balance between two processes: bone formation by osteoblasts and bone resorption by osteoclasts. In healthy individuals, these processes maintain bone strength and density. However, in osteoporosis, this balance is disrupted—osteoclast activity accelerates, breaking down bone tissue faster than osteoblasts can rebuild it. This imbalance leads to gradual thinning of bones and loss of structural integrity. Factors such as hormonal changes, aging, and certain medications exacerbate this process. Understanding bone remodeling is crucial because it explains why treatments often target osteoclast activity to slow bone loss. Drugs like bisphosphonates and denosumab work by inhibiting resorption, restoring some equilibrium and reducing fracture risk.
12. Economic Burden
Osteoporosis is not only a health issue but also a significant economic challenge. In the United States alone, osteoporosis-related fractures cost approximately $17 billion annually, and this figure is projected to soar to $50 billion by 2040 as the population ages. These costs include hospitalizations, surgeries, rehabilitation, and long-term care for patients who lose independence after fractures. Beyond direct medical expenses, osteoporosis imposes indirect costs such as lost productivity and caregiver burden. The financial impact rivals or exceeds that of other major chronic diseases like breast cancer and diabetes, highlighting the urgent need for preventive strategies and cost-effective treatments.
13. Hip Fracture Mortality
Hip fractures are among the most severe consequences of osteoporosis, often resulting in life-threatening complications. Nearly 20% of patients die within one year of sustaining a hip fracture, primarily due to infections, blood clots, and reduced mobility leading to systemic decline. Even survivors face long-term challenges—many never regain full independence and require permanent assistance or nursing home care. This high mortality rate underscores the importance of fall prevention and early osteoporosis management. It also illustrates how a seemingly localized injury can trigger a cascade of health problems, making hip fracture prevention a top priority in geriatric care.
14. Global Impact
Osteoporosis is a worldwide health concern, affecting an estimated 75 million people across the U.S., Europe, and Japan. In the United States alone, about 30 million individuals have low bone density, placing them at risk for future fractures. The global burden is expected to rise as life expectancy increases, particularly in developing countries where awareness and screening programs are limited. This widespread prevalence makes osteoporosis a critical focus for international health organizations, which advocate for education, early detection, and access to affordable treatments. The global scale of the disease emphasizes that osteoporosis is not just an individual problem—it is a societal challenge requiring coordinated action.
15. Lifestyle Prevention
Preventing osteoporosis begins with lifestyle choices that support bone health. Weight-bearing exercises such as walking, jogging, and resistance training stimulate bone formation and maintain density. Adequate intake of calcium and vitamin D is essential for bone mineralization, while smoking cessation and limiting alcohol consumption reduce risk factors that accelerate bone loss. These preventive measures are most effective when adopted early in life, but they remain beneficial even for older adults. Public health campaigns often stress these habits because they are simple, cost-effective, and have additional benefits for overall health. Lifestyle prevention is the cornerstone of osteoporosis management, complementing medical treatments and reducing long-term healthcare costs.
16. Medication Options
Pharmacological treatment for osteoporosis has evolved significantly over the past few decades, offering multiple options to slow bone loss and reduce fracture risk. The most commonly prescribed drugs are bisphosphonates, which inhibit osteoclast activity and prevent excessive bone resorption. These medications, such as alendronate and risedronate, are often the first line of defense for postmenopausal women and older men. Another class of drugs includes denosumab, a monoclonal antibody that targets RANKL, a protein essential for osteoclast formation. Hormone-related therapies, such as selective estrogen receptor modulators (SERMs) and hormone replacement therapy, are also used in specific cases. Newer treatments like teriparatide, a synthetic parathyroid hormone, stimulate bone formation rather than just slowing resorption. These medications have transformed osteoporosis management, but they require careful monitoring due to potential side effects, such as gastrointestinal issues or rare complications like osteonecrosis of the jaw.
17. Fall Prevention
Preventing falls is one of the most critical strategies for reducing fracture risk in individuals with osteoporosis. Even minor falls can result in severe injuries due to fragile bones. Fall prevention involves a multifaceted approach, including home safety modifications such as installing grab bars, removing loose rugs, and improving lighting. Balance and strength training exercises, like tai chi or yoga, help enhance stability and reduce the likelihood of falls. Vision checks and proper footwear also play a role in minimizing hazards. For older adults, assistive devices like canes or walkers may be necessary. Healthcare providers often emphasize fall prevention as much as medication because fractures from falls can lead to long-term disability, hospitalization, and even increased mortality.
18. Nutritional Factors
Nutrition is a cornerstone of bone health, and deficiencies in key nutrients can accelerate osteoporosis progression. Calcium and vitamin D are essential for bone mineralization, with recommended daily intakes varying by age and gender. Vitamin D facilitates calcium absorption, making it indispensable for skeletal strength. However, certain dietary habits can undermine bone health—excessive salt, caffeine, and alcohol intake increase calcium excretion, weakening bones over time. Protein is also vital, but extremely low or high protein diets can negatively affect bone metabolism. Maintaining a balanced diet rich in dairy products, leafy greens, and fortified foods is crucial for preventing osteoporosis. In cases where dietary intake is insufficient, supplements may be recommended, though they should be taken under medical supervision to avoid complications like kidney stones.
19. Interaction of Supplements
While supplements can help maintain bone health, improper combinations can reduce their effectiveness. A common example is the interaction between calcium and iron. Calcium interferes with iron absorption, meaning these two supplements should not be taken together. This is particularly important for individuals managing both osteoporosis and anemia. Healthcare providers often advise spacing these supplements several hours apart to ensure optimal absorption. Similarly, excessive intake of certain vitamins and minerals can lead to toxicity or imbalances that harm overall health. Understanding these interactions is essential for safe and effective supplementation, highlighting the importance of personalized guidance rather than self-prescription.
20. Types of Osteoporosis
Osteoporosis is classified into two main types: primary and secondary. Primary osteoporosis includes postmenopausal (Type I) and senile (Type II) forms. Postmenopausal osteoporosis occurs due to estrogen deficiency, leading to rapid bone loss in women after menopause. Senile osteoporosis affects both men and women over the age of 70 and is often linked to age-related declines in calcium absorption and vitamin D metabolism. Secondary osteoporosis, on the other hand, results from underlying medical conditions or medications, such as endocrine disorders, chronic kidney disease, or prolonged corticosteroid use. This classification is important because it guides treatment strategies—addressing the root cause in secondary osteoporosis can significantly improve outcomes, while primary osteoporosis often requires long-term management focused on slowing bone loss.
21. Senile Osteoporosis
Senile osteoporosis, also known as Type II osteoporosis, primarily affects individuals over the age of 70 and is often linked to age-related physiological changes. Unlike postmenopausal osteoporosis, which is driven by hormonal shifts, senile osteoporosis results from a gradual decline in calcium absorption and vitamin D metabolism. These changes reduce bone mineralization and compromise skeletal strength. Both men and women are susceptible, though men tend to develop it later in life. Senile osteoporosis often coexists with other age-related conditions, such as frailty and reduced mobility, compounding the risk of falls and fractures. Preventive strategies include maintaining adequate nutrition, engaging in weight-bearing exercise, and regular bone density screening to detect early signs of bone loss.
22. Postmenopausal Osteoporosis
Postmenopausal osteoporosis, or Type I osteoporosis, is one of the most common forms of the disease and occurs due to a sharp decline in estrogen levels after menopause. Estrogen plays a vital role in regulating bone remodeling by inhibiting osteoclast activity, which breaks down bone tissue. When estrogen levels drop, bone resorption accelerates, leading to rapid bone loss in women during the first decade after menopause. This type of osteoporosis primarily affects trabecular bone, found in the spine and wrist, making these areas particularly vulnerable to fractures. Hormone replacement therapy and medications like bisphosphonates are often prescribed to slow this process, alongside lifestyle interventions such as calcium and vitamin D supplementation.
23. Bone Density Testing
Bone density testing is a cornerstone of osteoporosis prevention and diagnosis. The most widely used method is the DEXA scan, which measures bone mineral density and provides a T-score to assess fracture risk. Guidelines recommend routine screening for women over 65 and men over 70, as well as earlier testing for individuals with risk factors such as previous fractures, long-term steroid use, or family history of osteoporosis. Early detection through bone density testing enables timely intervention, reducing the likelihood of debilitating fractures. These tests are quick, non-invasive, and widely available, making them an essential tool in public health strategies aimed at combating osteoporosis.
24. World Osteoporosis Day
World Osteoporosis Day, observed annually on October 20, is a global initiative led by the International Osteoporosis Foundation to raise awareness about bone health and fracture prevention. The campaign emphasizes education on risk factors, lifestyle changes, and the importance of early screening. Activities include public seminars, social media outreach, and collaborations with healthcare organizations to promote bone health worldwide. This day serves as a reminder that osteoporosis is a preventable condition and that proactive measures can significantly reduce its impact. By fostering global awareness, World Osteoporosis Day helps drive policy changes and funding for research and treatment programs.
25. No Complete Cure
Despite advances in medical science, there is currently no complete cure for osteoporosis. However, the condition can be effectively managed through a combination of lifestyle modifications, nutritional support, and pharmacological treatments. These interventions aim to slow bone loss, improve bone strength, and reduce fracture risk. While medications like bisphosphonates and denosumab can stabilize bone density, they do not restore it to youthful levels. This reality underscores the importance of prevention—building strong bones early in life and maintaining healthy habits throughout adulthood. With proper management, individuals with osteoporosis can lead active, fulfilling lives, but vigilance and adherence to treatment plans remain essential.
Frequently Asked Questions About Osteoporosis
1. What is osteoporosis?
Osteoporosis is a chronic condition where bones become weak and brittle due to loss of bone mass and structural deterioration. This makes them prone to fractures even from minor falls or simple movements like bending or coughing. It’s often called a “silent disease” because it progresses without symptoms until a fracture occurs. [mayoclinic.org]
2. What are the early symptoms of osteoporosis?
Most people have no symptoms in the early stages. As the disease advances, signs may include back pain from vertebral fractures, loss of height, stooped posture, and bones that break more easily than expected. [mayoclinic.org]
3. Who is at highest risk for osteoporosis?
Women—especially postmenopausal—are at greatest risk due to estrogen loss. Other risk factors include advanced age, family history, low body weight, smoking, excessive alcohol use, sedentary lifestyle, and certain medical conditions like rheumatoid arthritis or chronic kidney disease. [uconnhealth.org]
4. How is osteoporosis diagnosed?
The gold standard is a DEXA scan (Dual-energy X-ray absorptiometry), which measures bone mineral density. A T-score of −2.5 or lower indicates osteoporosis, while −1.0 to −2.4 suggests osteopenia (early bone loss). [communityh…clinic.org]
5. What is the difference between osteoporosis and osteopenia?
Osteopenia is a milder form of bone loss, with a T-score between −1.0 and −2.4. Osteoporosis is more severe, with a T-score of −2.5 or lower. Both conditions increase fracture risk, but osteoporosis carries a much higher risk. [mcpress.ma…clinic.org]
6. How often should I get a bone density test?
Women over 65 and men over 70 should have routine bone density testing. Younger individuals with risk factors—such as previous fractures or long-term steroid use—should be screened earlier. [aafp.org]
7. Can osteoporosis be prevented?
Yes. Prevention strategies include:
- Adequate calcium and vitamin D intake.
- Regular weight-bearing and resistance exercises.
- Avoiding smoking and excessive alcohol.
- Maintaining a healthy weight and active lifestyle. [mayoclinic.org]
8. What foods are best for bone health?
Calcium-rich foods like dairy products, leafy greens, and fortified cereals are essential. Vitamin D sources include fatty fish, eggs, and fortified milk. Limit salt, caffeine, and alcohol, as they can increase calcium loss. [drugs.com]
9. What medications are used to treat osteoporosis?
Common treatments include:
- Bisphosphonates (alendronate, risedronate).
- Denosumab (Prolia) for those who cannot tolerate bisphosphonates.
- Anabolic agents like teriparatide for severe cases. These drugs slow bone loss or stimulate bone formation. [mayoclinic.org]
10. How long do I need to take osteoporosis medication?
Treatment duration varies. Bisphosphonates are often taken for 3–5 years, followed by reassessment. Denosumab requires continuous use until transitioned to another drug, as stopping abruptly can increase fracture risk. [mayoclinic.org]
11. Are there side effects of osteoporosis medications?
Yes. Bisphosphonates can cause stomach upset and heartburn if not taken properly. Rare complications include osteonecrosis of the jaw and atypical femur fractures. Denosumab may increase infection risk. [uconnhealth.org]
12. Can osteoporosis be reversed?
There is no complete cure, but bone loss can be slowed or partially reversed with medication, lifestyle changes, and proper nutrition. Early intervention is key to preventing fractures. [drugs.com]
13. What exercises are safe for osteoporosis?
Weight-bearing activities like walking, light jogging, and resistance training are recommended. Balance exercises such as tai chi help prevent falls. Avoid high-impact or twisting movements if you have severe osteoporosis. [mayoclinic.org]
14. Is osteoporosis hereditary?
Yes, genetics play a role. If a parent had osteoporosis or hip fractures, your risk is higher. Family history should be considered when deciding on early screening. [osc-ortho.com]
15. What is the difference between osteoporosis and osteoarthritis?
Osteoporosis affects bone density, making bones fragile. Osteoarthritis affects joints, causing cartilage breakdown and pain. Both conditions can coexist but require different treatments. [drugs.com]
16. How dangerous are hip fractures caused by osteoporosis?
Hip fractures are serious, often requiring surgery and long recovery. About 20% of patients die within one year due to complications like infections and immobility. [aafp.org]
17. What role does vitamin D play in osteoporosis prevention?
Vitamin D helps the body absorb calcium, essential for bone strength. Deficiency increases fracture risk. Recommended intake is 800–1000 IU daily for adults over 50. [communityh…clinic.org]
18. Can men get osteoporosis?
Yes. Although less common than in women, men—especially over 70 or with low testosterone—are at risk. Screening and prevention are equally important for men. [aafp.org]
19. What is a T-score and why is it important?
A T-score compares your bone density to that of a healthy young adult. Normal: −1.0 or higher; Osteopenia: −1.0 to −2.4; Osteoporosis: −2.5 or lower. It helps determine fracture risk and treatment needs. [medicalnewstoday.com]
20. Are there natural treatments for osteoporosis?
Lifestyle changes—exercise, diet, and supplements—are the foundation. While some herbal remedies are marketed for bone health, none are proven as effective as medical treatments. Always consult your doctor before using alternatives. [drugs.com]