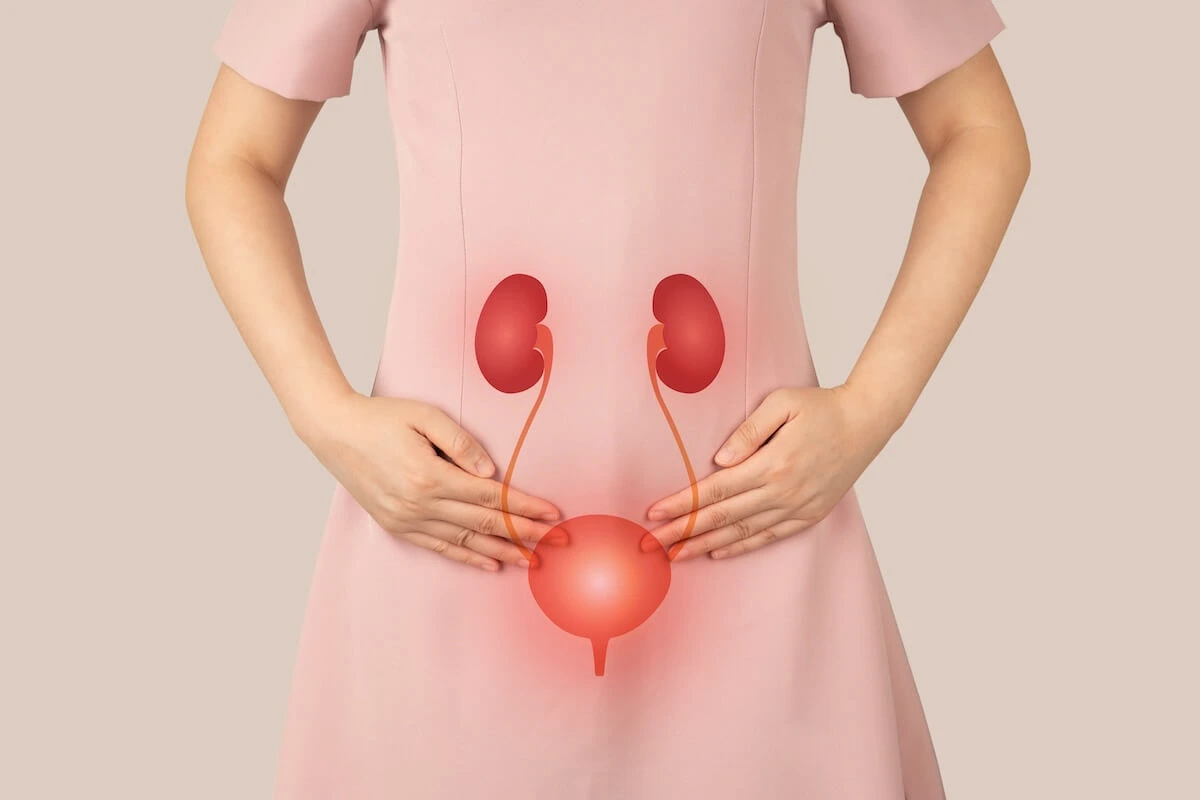
The human bladder is a muscular sac that holds urine. The bladder is a hollow organ composed of smooth muscle tissue known as the detrusor muscle. This muscle allows the bladder to expand as it fills with urine and contract to expel urine during urination. The bladder’s primary function is to store urine produced by the kidneys until it is convenient to eliminate it from the body, making it an essential component of the urinary system.
An average adult bladder can hold about 400 to 600 milliliters of urine. The bladder’s capacity can vary among individuals, but typically, it can comfortably hold between 400 to 600 milliliters (ml) of urine. When the bladder reaches its capacity, stretch receptors in the bladder wall signal the brain, creating the sensation of urgency to urinate. This capacity can be influenced by factors such as hydration levels, age, and individual bladder health.
The bladder is located in the pelvic cavity, behind the pubic bone. Anatomically, the bladder is situated in the pelvic cavity, specifically behind the pubic symphysis, which is the joint connecting the two halves of the pelvis. This positioning allows it to be supported by surrounding structures, including the pelvic floor muscles. The pelvic cavity’s anatomy plays a crucial role in the bladder’s function and its ability to expand and contract without causing discomfort.
The bladder wall is made up of a specialized tissue called transitional epithelium, which can stretch. The innermost layer of the bladder wall consists of transitional epithelium, a unique type of tissue that can stretch and change shape as the bladder fills. This ability is essential for the bladder’s function, as it allows the organ to accommodate varying volumes of urine without tearing or damage. The transitional epithelium also acts as a barrier to prevent urine from leaking into the surrounding tissues.
The average person urinates 6 to 8 times a day. On average, a healthy adult typically urinates between 6 to 8 times per day, depending on factors such as fluid intake, activity level, and overall health. This frequency is considered normal and indicates a properly functioning urinary system. However, some individuals may experience variations in urination frequency due to factors like hydration, medications, or medical conditions affecting the bladder.
The bladder is controlled by the autonomic nervous system and the somatic nervous system. The bladder’s function is regulated by both the autonomic nervous system, which controls involuntary actions, and the somatic nervous system, which governs voluntary actions. The autonomic nervous system manages the bladder’s filling and emptying reflexes, while the somatic nervous system allows for conscious control over urination. This dual control is essential for maintaining bladder health and function.
The urge to urinate typically occurs when the bladder fills to about 200 to 300 milliliters. As the bladder fills with urine, stretch receptors in the bladder wall send signals to the brain, creating the sensation of urgency. This urge usually begins when the bladder contains approximately 200 to 300 milliliters of urine. The sensation can vary in intensity based on individual sensitivity, bladder health, and other factors, influencing how quickly one responds to the urge.
The bladder can expand and contract due to its elastic properties. The bladder’s unique structure allows it to expand significantly as it fills with urine, accommodating volumes up to 600 milliliters or more. The detrusor muscle contracts during urination, pushing urine out through the urethra. This ability to stretch and contract is vital for the bladder’s role in urine storage and elimination, ensuring that it can function effectively over time.
In females, the bladder is shorter and located closer to the vagina than in males. Anatomically, the female bladder is positioned differently than the male bladder due to the differences in pelvic anatomy. In females, the bladder is typically shorter and located closer to the vagina, while in males, it is positioned higher and further from the urethra. This anatomical difference can influence the prevalence of urinary tract infections and other bladder-related issues between genders.
The bladder is connected to the kidneys via the ureters, which transport urine. The ureters are two slender tubes that connect the kidneys to the bladder, transporting urine produced by the kidneys for storage. Each ureter is approximately 25 to 30 centimeters (10 to 12 inches) long and uses peristaltic movements to propel urine downward. This connection is essential for the urinary system’s functioning, allowing for the continuous flow of urine from the kidneys to the bladder.
The urinary sphincter controls the release of urine from the bladder. The urinary sphincter is a circular muscle located at the base of the bladder that plays a critical role in controlling urination. There are two types of sphincters involved: the internal sphincter, which is involuntary and located at the junction of the bladder and urethra, and the external sphincter, which is voluntary and allows conscious control over urination. This dual control enables individuals to hold urine until they find an appropriate time and place to void.
Bladder infections, or cystitis, are more common in women than men. Cystitis, commonly referred to as a bladder infection, occurs when bacteria enter the bladder and cause inflammation. Women are more susceptible to bladder infections due to their shorter urethra, which allows bacteria easier access to the bladder. Factors such as sexual activity, certain contraceptive methods, and hormonal changes can also increase the risk of urinary tract infections (UTIs) in women, making awareness and preventive measures important.
The average bladder capacity can decrease with age. As people age, various physiological changes can occur, including a decrease in bladder capacity. Older adults may experience a reduction in the elasticity of the bladder wall and changes in the detrusor muscle’s function, which can lead to a decreased ability to store urine. This can result in more frequent urination and a higher likelihood of urinary incontinence, making it essential for older adults to manage their bladder health proactively.
The bladder can be affected by conditions such as overactive bladder and urinary incontinence. Overactive bladder (OAB) is a condition characterized by an urgent need to urinate, often accompanied by increased frequency and nocturia (waking up at night to urinate). Urinary incontinence refers to the involuntary leakage of urine, which can result from various factors, including weakened pelvic floor muscles, neurological disorders, or bladder dysfunction. Both conditions can significantly impact quality of life, and effective management strategies are available.
The bladder can also store urine for several hours without damage. The bladder is designed to store urine safely for several hours, allowing individuals to go about their daily activities without the constant need to urinate. The transitional epithelium lining the bladder provides a protective barrier against the acidic nature of urine, preventing damage to surrounding tissues. This storage capability is crucial for maintaining fluid balance and ensuring that the body can eliminate waste at appropriate times.
The first known description of the bladder dates back to ancient Egypt. Historical records indicate that the bladder has been recognized and studied for thousands of years, with one of the earliest known descriptions found in ancient Egyptian medical texts. These texts highlight the importance of the bladder and urinary system in health and disease. Ancient civilizations often attributed various functions to the bladder, demonstrating its significance in medical practices throughout history.
The bladder is lined with a mucous membrane that protects it from urine’s acidity. The bladder’s inner lining consists of a mucous membrane that secretes mucus to provide a protective barrier against the potentially irritating effects of urine. This mucus layer helps to prevent damage to the bladder wall and reduces the risk of infection. Additionally, the bladder’s unique epithelial cells can adapt to changes in urine composition, contributing to its overall health and function.
The bladder can be affected by lifestyle factors such as fluid intake and diet. Various lifestyle factors can influence bladder health, including fluid intake, diet, and habits. For instance, excessive caffeine or alcohol consumption may irritate the bladder and increase urgency and frequency of urination. Conversely, staying well-hydrated is essential for maintaining bladder function and preventing urinary tract infections. Individuals may need to adjust their fluid intake and dietary choices to support optimal bladder health.
The bladder plays a crucial role in the body’s waste elimination system. As a key component of the urinary system, the bladder’s primary function is to store and eliminate waste products filtered from the blood by the kidneys. This process is vital for maintaining the body’s fluid balance, electrolyte levels, and overall homeostasis. The bladder’s ability to store urine until it can be safely expelled ensures that the body effectively removes waste while preventing dehydration.
Bladder cancer is one of the most common types of urinary tract cancers. Bladder cancer originates in the bladder’s epithelial cells and can manifest in various forms, with transitional cell carcinoma being the most prevalent type. Risk factors for bladder cancer include smoking, exposure to certain chemicals, and chronic bladder inflammation. Early detection and treatment are crucial for improving outcomes, making awareness of symptoms such as blood in urine and frequent urination essential for timely medical intervention.
The bladder can be examined through a procedure called cystoscopy. Cystoscopy is a diagnostic procedure that allows healthcare providers to visualize the inside of the bladder and urethra using a thin, flexible tube called a cystoscope. This instrument is equipped with a camera and light, enabling doctors to detect abnormalities such as tumors, stones, or signs of infection. Cystoscopy is often performed when patients experience unexplained urinary symptoms, and it can also be used for therapeutic purposes, such as removing stones or taking biopsies.
The bladder can be affected by neurological disorders, impacting its function. Neurological disorders such as multiple sclerosis, Parkinson’s disease, and spinal cord injuries can significantly impact bladder function. These conditions may disrupt the nerve signals that control bladder contraction and relaxation, leading to issues such as urinary incontinence, urgency, or retention. Management of bladder dysfunction in patients with neurological disorders often requires a multidisciplinary approach, including medications, bladder training, and sometimes surgical interventions.
The bladder has a unique ability to signal the brain when it is full. As the bladder fills with urine, stretch receptors in the bladder wall become activated and send signals to the brain indicating fullness. This communication is crucial for maintaining bladder health, as it prompts the individual to seek a restroom when necessary. The brain processes these signals and can override them, allowing for voluntary control over urination. This complex interaction between the bladder and the brain is essential for normal urinary function.
The bladder can be artificially created in certain medical procedures, such as bladder reconstruction. In cases where the bladder is severely damaged or removed due to disease, such as cancer, surgeons can create a new bladder from a portion of the intestine in a procedure known as bladder reconstruction or neobladder formation. This artificial bladder can function similarly to a natural bladder, allowing the patient to store and eliminate urine. This surgical option can significantly enhance the quality of life for individuals who have undergone bladder removal.
The bladder’s function is essential for maintaining the body’s fluid balance. The bladder plays a critical role in the body’s overall fluid balance by storing urine until it can be safely expelled. This function helps regulate the body’s hydration levels and electrolyte balance, which are vital for numerous physiological processes. By controlling when and how much urine is eliminated, the bladder helps prevent both dehydration and fluid overload, contributing to the body’s homeostasis and overall health.
Here are some common FAQs about the bladder, answered in detail:
1. What is the bladder, and what does it do?
The bladder is a hollow, muscular organ located in your pelvis. Its primary function is to store urine, a liquid waste product produced by your kidneys. As urine is produced, it flows from the kidneys through tubes called ureters and into the bladder. The bladder expands to accommodate increasing amounts of urine. When it reaches a certain capacity, nerve signals are sent to the brain, triggering the urge to urinate.
2. What are some common bladder problems?
Several common bladder problems can affect people of all ages. Here are a few:
- Overactive Bladder (OAB): This condition causes a frequent and urgent need to urinate, often leading to accidents.
- Urinary Incontinence: This involves the involuntary leakage of urine. It can be stress incontinence (leakage during physical activity), urge incontinence (sudden, uncontrollable urges), or mixed incontinence (a combination of both).
- Urinary Tract Infection (UTI): A bacterial infection that affects the urinary tract, often causing pain, burning, and frequent urination.
- Interstitial Cystitis (IC): A chronic bladder condition that causes pelvic pain and frequent urination.
3. How can I improve my bladder health?
Here are some tips to maintain a healthy bladder:
- Drink plenty of water: While it may seem counterintuitive, staying hydrated can help prevent urinary tract infections and improve bladder function.
- Limit caffeine and alcohol: These substances can irritate the bladder and worsen symptoms of bladder conditions.
- Practice pelvic floor exercises: Kegel exercises can strengthen the pelvic floor muscles, which support the bladder and urethra.
- Maintain a healthy weight: Excess weight can put pressure on the bladder and contribute to incontinence.
- Avoid constipation: Constipation can put pressure on the bladder and worsen urinary symptoms.
- Time your bathroom trips: Try to establish a regular bathroom schedule and avoid holding urine for too long.
- Consider bladder training: This involves gradually increasing the time between bathroom trips to improve bladder control.
4. When should I see a doctor about bladder problems?
You should consult a doctor if you experience any of the following:
- Frequent or urgent urination
- Painful urination
- Blood in your urine
- Incontinence
- Difficulty urinating
- A persistent urge to urinate but little urine comes out
5. What are the treatment options for bladder problems?
Treatment for bladder problems depends on the specific condition and its severity. Some common treatment options include:
- Lifestyle modifications: Changes in diet, fluid intake, and bladder habits.
- Pelvic floor therapy: Exercises to strengthen the pelvic floor muscles.
- Medication: To treat symptoms of overactive bladder, urinary incontinence, or UTIs.
- Bladder training: A behavioral therapy to help improve bladder control.
- Surgery: In severe cases, surgery may be necessary to correct underlying anatomical issues or remove bladder tumors.
If you have concerns about your bladder health, it’s important to consult a healthcare professional for proper diagnosis and treatment.