Sleep apnea is far more than just loud snoring—it’s a serious medical condition that affects millions of people worldwide, often without their knowledge. Characterized by repeated interruptions in breathing during sleep, sleep apnea can lead to a host of health problems, including heart disease, diabetes, and depression. Despite its prevalence, many cases remain undiagnosed, and public awareness is still catching up to the science. In this blog, we uncover 25 fascinating and verified facts about sleep apnea—from surprising statistics and historical milestones to cutting-edge technology and life-saving treatments. Whether you’re newly diagnosed, supporting a loved one, or simply curious, these insights will deepen your understanding of this complex and often overlooked sleep disorder.
1. 30 Million Americans Have Sleep Apnea
An estimated 30 million adults in the United States suffer from obstructive sleep apnea (OSA), according to the American Medical Association. This staggering number reflects how widespread the condition is, yet many individuals remain unaware of their diagnosis. Symptoms such as daytime fatigue, mood swings, and increased risk of chronic illnesses often go unnoticed or misattributed. Lofta’s at-home sleep tests aim to bridge this gap by making diagnosis more accessible and convenient.
2. 80% of Moderate and Severe OSA Cases Are Undiagnosed
Despite its prevalence, 80% of moderate to severe sleep apnea cases go undiagnosed. This is largely due to the subtlety of symptoms like snoring, restless sleep, or waking up tired, which people often dismiss. Untreated sleep apnea can lead to serious complications including heart disease, stroke, and diabetes, making early screening and awareness critically important.
3. Men Are 2 to 3 Times More Likely to Develop OSA
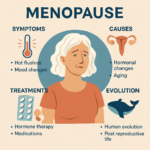
Men are 2 to 3 times more likely to develop sleep apnea than women, especially between the ages of 30 and 50. This is due to anatomical differences and hormonal factors that affect airway stability. However, post-menopausal women experience a sharp increase in risk, highlighting the need for gender-specific screening and awareness as people age.
4. CPAP Therapy Lowers Blood Pressure
Continuous Positive Airway Pressure (CPAP) therapy has been clinically proven to reduce high blood pressure in patients with sleep apnea. By keeping the airway open and improving oxygen flow during sleep, CPAP not only enhances sleep quality but also supports cardiovascular health, reducing the risk of hypertension-related complications.
5. OSA Increases Stroke Risk by Up to 3 Times
Individuals with untreated sleep apnea face a two to threefold increased risk of stroke. The repeated drops in oxygen levels during sleep strain the circulatory system, increasing the likelihood of blood clots and vascular damage. CPAP therapy helps stabilize breathing and oxygenation, significantly lowering this risk.
6. 50% of Type 2 Diabetics Have Sleep Apnea
Studies show that 50% of people with Type 2 diabetes also suffer from sleep apnea. Poor sleep quality worsens insulin resistance, making blood sugar management more difficult. Treating sleep apnea can improve metabolic function and help diabetics maintain better control over their condition.
7. OSA Raises the Risk of Heart Failure
Sleep apnea places significant strain on the heart due to repeated oxygen deprivation. Over time, this can lead to heart failure, especially in individuals with existing cardiovascular conditions. CPAP therapy mitigates this risk by ensuring consistent oxygen levels and reducing nighttime stress on the heart.
8. CPAP Reduces the Risk of Car Accidents
Daytime sleepiness caused by sleep apnea is a major contributor to drowsy-driving accidents. CPAP therapy restores restful sleep, improving alertness and reaction time. Commercial drivers and shift workers report feeling significantly safer and more focused after starting CPAP treatment.
9. Sleep Apnea Costs the U.S. $150 Billion Annually
Untreated sleep apnea contributes to an estimated $150 billion in annual costs in the U.S., including healthcare expenses, lost productivity, and accident-related damages. Investing in early diagnosis and treatment can dramatically reduce this financial burden and improve public health outcomes.
10. Obesity Is the Strongest Risk Factor for OSA
Between 60–90% of adults with sleep apnea are overweight or obese. Excess fat around the neck and chest compresses the airway, increasing the likelihood of breathing interruptions. Weight loss, combined with CPAP therapy, can significantly improve symptoms and overall health.
11. Post-Menopausal Women Are at High Risk
Although sleep apnea is less common in women, the risk rises sharply after menopause. Hormonal changes affect muscle tone in the airway, making it more prone to collapse during sleep. Women over 50 should consider regular screening, especially if they experience symptoms like snoring or fatigue.
12. CPAP Compliance Lowers Hospital Readmission Rates
Patients who consistently use CPAP therapy after surgery or hospitalization are less likely to be readmitted. Improved oxygenation and sleep quality support faster recovery and reduce complications, making CPAP a valuable tool in post-operative care and chronic disease management.
13. OSA Is Linked to Higher Depression Rates
Sleep apnea is closely associated with depression and anxiety. Interrupted sleep affects brain chemistry and emotional regulation. Studies show that CPAP therapy often leads to noticeable improvements in mood and mental health within just a few weeks of consistent use.
14. CPAP Users Report Increased Quality of Life
Beyond medical benefits, CPAP users report better energy levels, concentration, and relationship satisfaction. Many experience a dramatic improvement in overall well-being, including reduced irritability and enhanced productivity, after starting therapy.
15. 20% of Obese Children Have Sleep Apnea
Sleep apnea affects 1 in 5 obese children, leading to disrupted sleep, poor academic performance, and behavioral issues. Pediatric sleep apnea is often underdiagnosed but can be treated effectively with lifestyle changes, CPAP, or surgical interventions like tonsil removal.
16. CPAP Masks Are Now Designed for Maximum Comfort
Modern CPAP masks are lightweight, flexible, and engineered to minimize air leaks. These design improvements increase comfort and adherence, making long-term therapy more sustainable. Patients can choose from nasal, full-face, or nasal pillow masks based on their preferences.
17. Wearable Devices Are Improving OSA Detection
Smartwatches and fitness trackers now offer sleep apnea detection features, alerting users to abnormal breathing patterns. While not diagnostic, these tools encourage earlier medical evaluation and can be a helpful first step toward treatment.
18. Untreated OSA Can Worsen GERD Symptoms
Sleep apnea and gastroesophageal reflux disease (GERD) often co-exist. CPAP therapy can help stabilize the airway and esophagus, reducing acid reflux episodes during sleep. This dual benefit improves both respiratory and digestive health.
19. Portable CPAP Machines Revolutionize Travel
Compact CPAP devices now allow patients to maintain therapy while traveling. These portable machines are ideal for frequent flyers and vacationers, ensuring uninterrupted treatment and better sleep on the go.
20. At-Home Sleep Tests Are Highly Accurate
Devices like WatchPAT ONE offer reliable at-home sleep apnea testing, eliminating the need for overnight lab stays. These tests provide fast results and help patients begin treatment sooner, improving access to care.
21. Telehealth Is Transforming Sleep Apnea Care
Telehealth services now allow patients to receive CPAP prescriptions online, streamlining access to care. Remote consultations and digital monitoring are making sleep apnea treatment more accessible, especially in underserved areas.
22. OSA Affects 1 in 5 Adults Worldwide
Globally, 1 in 5 adults suffers from sleep apnea, making it a major public health issue. Increased awareness and affordable testing are essential to address this widespread condition and reduce its health burden.
23. CPAP Therapy Reduces Emergency Room Visits
By preventing serious complications, CPAP therapy helps reduce ER visits and hospitalizations, lowering healthcare costs and improving patient outcomes. This makes CPAP not only a health solution but also a cost-effective intervention.
24. Sleep Apnea Was First Identified in 1965
Sleep apnea was officially recognized in 1965, when researchers documented breathing pauses during sleep. This discovery led to decades of research and the development of modern treatments like CPAP, transforming sleep medicine.
25. The Future of Sleep Apnea Care Is Virtual
With advances in telemedicine, wearable tech, and home diagnostics, sleep apnea care is shifting toward virtual platforms. This evolution promises faster, more convenient access to life-changing treatment, especially for remote or busy patients.
Frequently Asked Questions about Sleep Apnea:
1. What is Sleep Apnea?
Sleep apnea is a sleep disorder characterized by repeated interruptions in breathing during sleep. These interruptions can be partial (hypopneas) or complete (apneas), and they occur when the airway collapses or becomes blocked. The most common type is Obstructive Sleep Apnea (OSA), where the soft tissues in the throat relax excessively, obstructing airflow. These breathing pauses can last 10 seconds or longer and may occur dozens to hundreds of times per night, leading to poor sleep quality and reduced oxygen levels.
2. Is it normal to stop breathing while sleeping?
No, it is not normal to stop breathing during sleep. While brief pauses in breathing can happen occasionally, frequent or prolonged interruptions are a sign of sleep apnea and should be evaluated by a healthcare provider. These episodes can lead to oxygen deprivation, fragmented sleep, and increased risk of serious health issues like high blood pressure, heart disease, and stroke.
3. Is snoring the same as sleep apnea?
Not necessarily. Snoring is a common symptom of sleep apnea but can also occur independently. Snoring is caused by turbulent airflow that vibrates the soft tissues in the airway. In sleep apnea, snoring is often accompanied by gasping, choking, or pauses in breathing, which are more concerning. A sleep study is the only way to determine whether snoring is related to sleep apnea.
4. What is a sleep study and how much does it cost?
A sleep study is a diagnostic test that monitors breathing, oxygen levels, heart rate, and other physiological functions during sleep. It can be conducted in a sleep lab (costing around $1,000) or at home using a Home Sleep Test (HST), which typically costs $200–$300. Insurance often covers part or all of the cost. In-lab studies provide more comprehensive data, including brain wave activity, while HSTs focus on breathing and oxygen levels and are best for diagnosing OSA.
5. What causes sleep apnea?
Sleep apnea can be caused by a combination of factors including airway structure, genetics, and weight. People with naturally narrow airways are more prone to obstruction during sleep. Obesity exacerbates this by adding pressure to the airway. Other contributing factors include large tonsils, nasal congestion, and muscle tone loss due to aging or hormonal changes. While weight loss can reduce severity, it doesn’t always cure sleep apnea.
6. Is sleep apnea genetic?
While there isn’t a specific “sleep apnea gene,” genetics play a role in airway anatomy. Individuals with a family history of sleep apnea are 50% more likely to develop the condition. Traits like a smaller airway or facial structure can be inherited, increasing the risk of airway collapse during sleep.
7. What problems does sleep apnea cause?
Untreated sleep apnea can lead to daytime fatigue, difficulty concentrating, and mood disturbances. In children, it may mimic symptoms of ADHD. Long-term complications include high blood pressure, heart arrhythmias, stroke, and diabetes. It can also worsen existing conditions like depression, anxiety, and migraines. Effective treatment significantly reduces these risks and improves overall health.
8. Can you die from sleep apnea?
While rare, death from sleep apnea can occur, usually due to complications like abnormal heart rhythms or cardiac arrest triggered by prolonged oxygen deprivation. Sleep apnea is a serious condition that should not be ignored. Proper treatment, such as CPAP therapy, can greatly reduce the risk of life-threatening events.
9. What cures sleep apnea?
There is no universal cure for sleep apnea. CPAP therapy is the most effective treatment for managing symptoms. In some cases, surgical removal of large tonsils or adenoids, or significant weight loss, may eliminate the condition. However, for most people, ongoing management with CPAP or other therapies is necessary to maintain healthy sleep and prevent complications.
10. How common is sleep apnea?
Sleep apnea is very common, affecting 20–30% of men and 10–15% of women in North America. The prevalence increases with age and weight. After menopause, women’s risk becomes equal to men’s due to hormonal changes that affect muscle tone in the airway. Despite its prevalence, many cases remain undiagnosed.