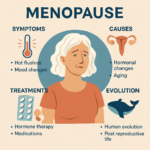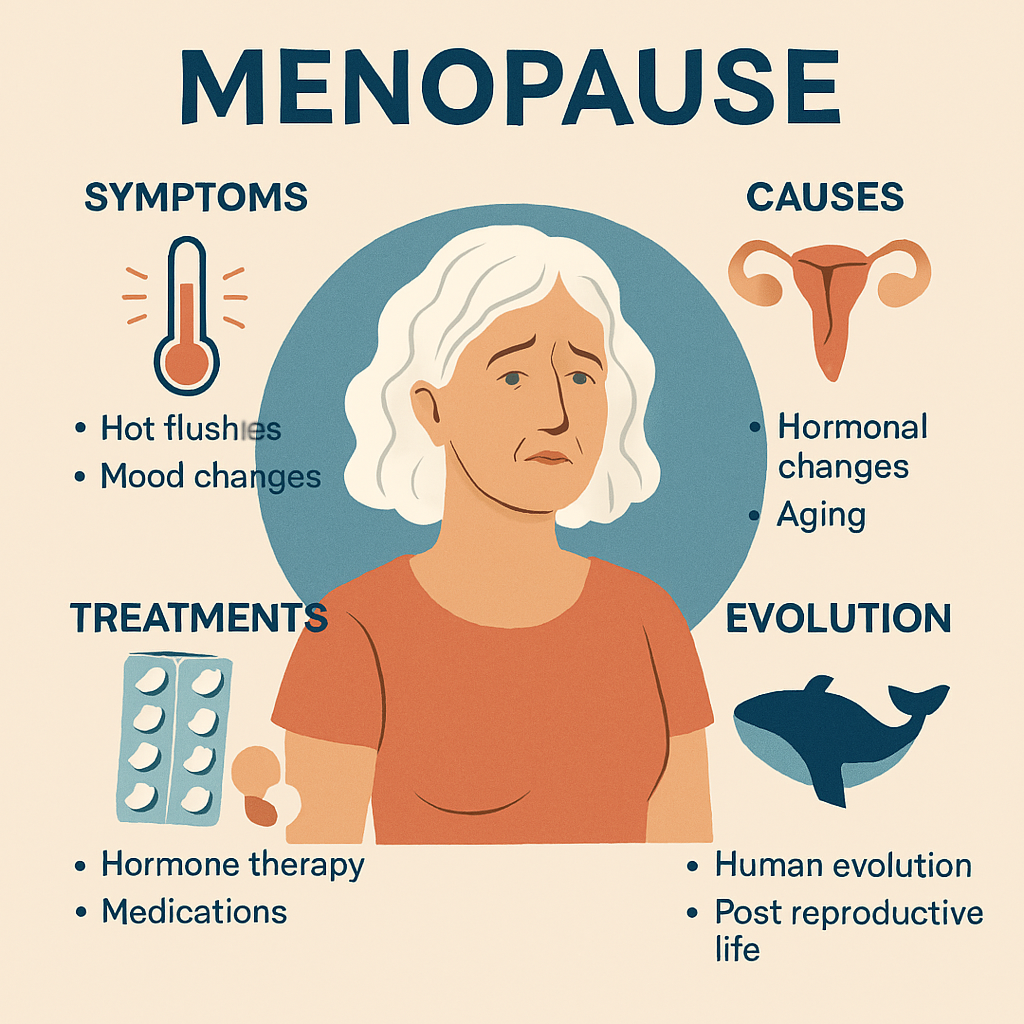
Menopause
Menopause is one of the most significant milestones in a woman’s life, yet it’s often surrounded by myths, misconceptions, and silence. Far from being just the “end of periods,” menopause is a complex biological transition that affects the body, mind, and even society in fascinating ways. From its evolutionary roots shared with whales, to the cultural perspectives that celebrate it as a time of wisdom and freedom, menopause is much more than a medical event — it’s a story of resilience, adaptation, and transformation.
In this post, we’ll explore 25 interesting facts about menopause that shed light on its science, symptoms, treatments, and cultural significance. Whether you’re approaching this stage yourself, supporting someone who is, or simply curious about how human biology works, these insights will help you see menopause in a whole new light.
🧬 Definition & Basics
1. Menopause is defined as 12 consecutive months without menstruation. Menopause is clinically diagnosed when a woman has not experienced a menstrual period for a full year, without other medical causes such as pregnancy or illness. This definition is important because menstrual cycles can become irregular during perimenopause, with skipped months or lighter bleeding, but these fluctuations alone do not qualify as menopause. The 12-month threshold ensures that ovarian activity has truly ceased, marking the end of reproductive capacity. This standardized definition helps doctors distinguish menopause from other gynecological conditions and provides a clear marker for when a woman has entered postmenopause.
2. The average age of menopause is 51 years. While menopause can occur anywhere between ages 45 and 55, the global average is around 51. This age reflects the natural decline in ovarian function and the depletion of viable eggs. Interestingly, the timing of menopause has remained relatively stable across generations, despite improvements in healthcare and life expectancy. Women today often live decades beyond menopause, which raises questions about the evolutionary role of this stage of life. The average age also varies slightly by ethnicity, lifestyle, and geography, with some populations experiencing menopause earlier or later.
3. The transition phase is called perimenopause. Perimenopause refers to the years leading up to menopause, when hormonal fluctuations begin to disrupt regular cycles. This phase can last anywhere from 2 to 10 years, and symptoms often start subtly, such as irregular periods, mood swings, or mild hot flashes. Estrogen and progesterone levels fluctuate unpredictably, sometimes causing heavier bleeding or skipped cycles. Perimenopause is often the most symptomatic stage, as the body struggles to adapt to declining hormone levels. Recognizing this phase is crucial, as many women seek medical support during perimenopause rather than after menopause itself.
4. Menopause is considered a natural biological process, not a disease. Although menopause can bring uncomfortable symptoms, it is not classified as a medical disorder. Instead, it is a natural stage of aging, much like puberty. This distinction is important because it shapes how society and medicine approach menopause: rather than “curing” it, the goal is to manage symptoms and support women through the transition. However, medicalization of menopause has been debated, especially with the widespread use of hormone therapy. Framing menopause as natural helps reduce stigma and emphasizes resilience, though it doesn’t diminish the need for effective treatments.
5. The duration of menopausal transition can range from 5–15 years. The journey from perimenopause to postmenopause is highly individual. Some women experience only a few years of mild symptoms, while others endure a decade or more of hot flashes, mood changes, and sleep disturbances. This variability is influenced by genetics, lifestyle, and health conditions. The long duration highlights why menopause is not a single event but a prolonged transition. Understanding this timeline helps women prepare for ongoing changes and encourages healthcare providers to offer sustained support rather than short-term fixes.
⚕️ Causes & Triggers
6. The most common cause is the natural decline of ovarian function. Menopause occurs because the ovaries gradually stop releasing eggs and producing hormones like estrogen and progesterone. This decline is part of the natural aging process, as women are born with a finite number of eggs that diminish over time. By midlife, the remaining eggs are insufficient to sustain regular cycles, and hormone production drops sharply. This hormonal decline is what drives most menopausal symptoms, from hot flashes to bone density loss. It is a universal biological process, though the exact timing varies.
7. Surgical removal of both ovaries can trigger immediate menopause. When both ovaries are surgically removed, usually due to cancer risk or other medical conditions, menopause occurs instantly, regardless of age. This is called “surgical menopause,” and it is often more severe than natural menopause because hormone levels plummet abruptly rather than gradually. Women who undergo surgical menopause may experience intense hot flashes, mood swings, and vaginal dryness within weeks. Because of the sudden onset, hormone therapy is often recommended to ease symptoms and protect bone and heart health.
8. Certain chemotherapy and radiation treatments can induce menopause. Cancer treatments that damage ovarian tissue can lead to premature menopause. Chemotherapy drugs, especially those targeting rapidly dividing cells, often harm the ovaries, while pelvic radiation can destroy ovarian function entirely. This treatment-induced menopause can occur at any age, sometimes in women as young as their 20s or 30s. The emotional impact is significant, as it may affect fertility and quality of life. Doctors often discuss fertility preservation before treatment, such as egg freezing, to help women prepare for this possibility.
9. Smoking is linked to earlier onset of menopause. Studies consistently show that women who smoke tend to reach menopause 1–2 years earlier than non-smokers. The toxins in cigarettes accelerate the loss of ovarian follicles and interfere with estrogen production. This earlier onset increases the risk of long-term health issues like osteoporosis and heart disease, since women spend more years in a low-estrogen state. Smoking also worsens menopausal symptoms, making hot flashes and sleep disturbances more severe. This link underscores the importance of lifestyle choices in reproductive health.
10. Genetics play a role in the timing of menopause. Family history strongly influences when menopause occurs. If a woman’s mother or sisters experienced early menopause, she is more likely to do so as well. Genetic factors regulate ovarian reserve and hormone production, determining how long the reproductive system remains active. Researchers have identified specific genes associated with ovarian aging, though the full picture is complex. This genetic influence explains why menopause timing varies widely among women, even when lifestyle factors are similar.
🌡️ Symptoms & Effects
11. Hot flashes are the most common symptom, affecting up to 75% of women. Hot flashes are sudden feelings of intense heat, often accompanied by sweating, flushing, and rapid heartbeat. They can last from seconds to several minutes and occur unpredictably, sometimes multiple times a day. The exact cause is linked to changes in the hypothalamus, the brain’s temperature regulator, which becomes more sensitive to hormonal fluctuations. Hot flashes can disrupt daily life and sleep, making them one of the most distressing symptoms. Their prevalence across cultures highlights their strong biological basis.
12. Night sweats and sleep disturbances are frequent complaints. Night sweats are hot flashes that occur during sleep, often soaking bedclothes and sheets. They disrupt rest and contribute to insomnia, fatigue, and irritability. Sleep disturbances may also stem from hormonal changes affecting melatonin and circadian rhythms. Poor sleep quality during menopause can worsen mood swings and cognitive function, creating a cycle of discomfort. Addressing sleep issues is a major focus of menopause management, with strategies ranging from cooling bedding to medical treatments.
13. Mood changes such as irritability, anxiety, or depression may occur. Hormonal fluctuations during menopause affect neurotransmitters like serotonin and dopamine, which regulate mood. As a result, many women experience increased irritability, anxiety, or even depression. These changes are compounded by sleep disturbances and the psychological impact of aging. While not all women develop mood disorders, the risk is higher during perimenopause. Recognizing these emotional shifts is important, as they can be misattributed to stress or external factors rather than hormonal changes.
14. Vaginal dryness and reduced libido are common physical effects. Declining estrogen levels cause thinning of vaginal tissues and reduced lubrication, leading to discomfort during intercourse. This condition, known as genitourinary syndrome of menopause (GSM), can also cause itching, burning, and urinary problems. Reduced libido may result from both physical discomfort and hormonal changes affecting sexual desire. These symptoms can strain relationships and self-esteem, but treatments like lubricants, vaginal estrogen, and counseling can help restore sexual health.
15. Long-term risks include osteoporosis and cardiovascular changes. Estrogen plays a crucial role in maintaining bone density and protecting heart health. After menopause, the decline in estrogen accelerates bone loss, increasing the risk of osteoporosis and fractures. Cardiovascular risks also rise, as estrogen helps regulate cholesterol and blood vessel function. Postmenopausal women are more prone to heart disease, making lifestyle changes and medical monitoring essential. These long-term risks highlight why menopause is not just about short-term symptoms but also about lifelong health management.
💊 Treatments & Management
16. Hormone therapy (HT) is the most effective treatment for hot flashes. HT involves replacing estrogen, sometimes combined with progesterone, to alleviate symptoms like hot flashes, night sweats, and vaginal dryness. It is the gold standard for symptom relief, but it carries risks, including increased chances of blood clots, breast cancer, and stroke. Doctors weigh these risks against benefits, tailoring therapy to individual needs. Short-term use at the lowest effective dose is often recommended. Despite controversies, HT remains a cornerstone of menopause management.
17. Non-hormonal medications include SSRIs, gabapentin, clonidine, and lisdexamfetamine. For women who cannot take hormones, alternatives exist. SSRIs (antidepressants) can reduce hot flashes and improve mood. Gabapentin, originally for seizures, helps with night sweats. Clonidine, a blood pressure medication, can ease hot flashes, though side effects limit its use. Lisdexamfetamine, used for ADHD, has shown promise in reducing hot flashes. These options expand treatment choices, ensuring women with contraindications to hormones still receive relief.
18. Lifestyle changes can ease symptoms. Lifestyle adjustments are often the first line of defense against menopausal discomfort. Regular exercise improves cardiovascular health, strengthens bones, and boosts mood by releasing endorphins. A balanced diet rich in calcium, vitamin D, and phytoestrogens (found in soy and flaxseed) can help reduce bone loss and ease hot flashes. Stress management techniques such as yoga, meditation, and deep breathing exercises are also effective in reducing anxiety and improving sleep quality. Avoiding triggers like caffeine, alcohol, and spicy foods can lessen hot flashes and night sweats. These changes not only alleviate symptoms but also promote long-term health, making lifestyle management a cornerstone of menopause care.
19. Phytoestrogens are sometimes used, though evidence is mixed. Phytoestrogens are plant-derived compounds that mimic estrogen in the body, found in foods like soy, chickpeas, and flaxseed. Some women turn to phytoestrogen supplements or diets to ease hot flashes and improve bone health. While certain studies suggest modest benefits, others show little to no effect, and results vary widely among individuals. The appeal lies in their natural origin and perceived safety compared to hormone therapy, but medical experts caution that phytoestrogens are not risk-free, especially in women with hormone-sensitive conditions. Their role remains controversial, highlighting the need for more research to clarify their effectiveness and safety.
20. Cognitive behavioral therapy (CBT) can help manage mood and sleep issues. CBT is a structured psychological treatment that helps women reframe negative thoughts and develop coping strategies. During menopause, CBT has been shown to reduce anxiety, depression, and insomnia by addressing the emotional and behavioral aspects of symptoms. For example, CBT can help women manage the distress caused by hot flashes by teaching relaxation techniques and reducing catastrophic thinking. It also improves sleep hygiene, helping women establish healthier bedtime routines. Unlike medication, CBT carries no physical side effects, making it a valuable tool for women seeking non-pharmacological support during menopause.
🌍 Evolutionary & Cultural Context
21. Humans are one of the few species with menopause. Menopause is rare in the animal kingdom. Besides humans, only certain whale species — including orcas, pilot whales, belugas, and narwhals — experience menopause. In these species, older females stop reproducing but continue to live long lives, often playing crucial roles in their social groups. This phenomenon suggests an evolutionary advantage, as post-reproductive females contribute to the survival of their kin by sharing knowledge, resources, and caregiving. The rarity of menopause across species makes it a fascinating subject of evolutionary biology, raising questions about why it developed in humans and whales but not in most other animals.
22. The “Grandmother hypothesis” suggests menopause evolved to allow older women to help raise grandchildren. This evolutionary theory argues that menopause exists because it enhances survival of offspring and grandchildren. By ceasing reproduction, older women can devote energy and resources to supporting their children and grandchildren, increasing the chances of family survival. Studies of hunter-gatherer societies show that grandmothers often play a vital role in food gathering and childcare, directly influencing the survival rates of grandchildren. This hypothesis explains why women live decades beyond their reproductive years, suggesting that menopause is not a biological flaw but an adaptive trait that benefits human communities.
23. In some cultures, menopause is viewed positively as a transition to wisdom and freedom. While Western societies often frame menopause negatively, focusing on symptoms and aging, many cultures see it as a liberating stage. In certain Indigenous and Asian traditions, menopause marks a woman’s transition into a respected elder role, free from the responsibilities of childbearing. Women may gain social authority, spiritual recognition, or leadership opportunities. This cultural perspective highlights how attitudes toward menopause are shaped by societal values. Viewing menopause as a time of empowerment rather than decline can improve psychological well-being and reduce stigma.
24. Historically, menopause was called the “climacteric.” The term “climacteric,” derived from Greek, means a critical period or turning point in life. In ancient medicine, menopause was seen as a natural but significant stage, often associated with changes in health and vitality. Early medical texts described it as a time when women became more prone to illness, reflecting limited understanding of hormonal changes. Over time, the term fell out of common use, replaced by “menopause” in the 19th century. The historical language surrounding menopause reveals how perceptions of aging and female biology have evolved across centuries.
25. The Menopause Society (formerly NAMS) was founded in 1989 to promote research and education. The Menopause Society, originally known as the North American Menopause Society (NAMS), was established to advance knowledge about midlife and aging in women. It provides guidelines for healthcare providers, supports scientific research, and educates the public about menopause management. The organization has played a key role in shaping medical practices, particularly regarding hormone therapy and alternative treatments. By fostering collaboration among doctors, researchers, and educators, the society ensures that women receive evidence-based care and accurate information. Its work underscores the importance of treating menopause as a major public health issue, not just a private experience.
🔎 Frequently Asked Questions About Menopause
1. What is menopause and when does it happen?
Menopause is the natural biological process marking the end of a woman’s reproductive years. It is diagnosed after 12 consecutive months without menstruation. The average age of menopause is around 51 years, though it typically occurs between 45–55 years. Factors such as genetics, smoking, and medical treatments can influence timing.
2. What are the stages of menopause?
Menopause is not a single event but a transition:
- Perimenopause: Begins several years before menopause, with irregular cycles and symptoms like hot flashes.
- Menopause: Officially diagnosed after 12 months without a period.
- Postmenopause: The years following menopause, when symptoms may ease but long-term health risks (osteoporosis, heart disease) increase.
3. What are the most common symptoms?
- Hot flashes and night sweats (vasomotor symptoms)
- Sleep disturbances and insomnia
- Mood changes such as irritability, anxiety, or depression
- Vaginal dryness and reduced libido
- Memory and concentration difficulties
- Bone loss and increased risk of osteoporosis
4. How is menopause diagnosed?
Most women recognize menopause by symptoms and menstrual changes. Blood tests are rarely needed but may check FSH (follicle-stimulating hormone) and estradiol levels. Elevated FSH and low estrogen suggest menopause. Doctors may also rule out thyroid disorders, which can mimic menopausal symptoms.
5. Can I still get pregnant during menopause?
During perimenopause, ovulation is irregular but still possible, meaning pregnancy can occur. Once menopause is confirmed (12 months without periods), natural pregnancy is no longer possible. However, assisted reproductive technologies (like donor eggs) remain an option.
6. What treatments are available for symptoms?
- Hormone Therapy (HT): The most effective treatment for hot flashes and vaginal dryness, but carries risks (blood clots, breast cancer).
- Non-hormonal medications: SSRIs, gabapentin, clonidine, and lisdexamfetamine can help with hot flashes and mood.
- Lifestyle changes: Exercise, healthy diet, stress management, and avoiding triggers like caffeine and alcohol.
- Alternative therapies: Phytoestrogens (soy, flaxseed) and herbal remedies, though evidence is mixed.
7. Is hormone therapy safe?
Hormone therapy is effective but not suitable for everyone. Risks include heart disease, stroke, and breast cancer, especially with long-term use. Doctors often recommend the lowest effective dose for the shortest duration. Women with a history of certain cancers or blood clots may be advised against HT.
8. What long-term health risks are associated with menopause?
- Osteoporosis: Estrogen decline accelerates bone loss.
- Cardiovascular disease: Higher risk of heart disease after menopause.
- Weight gain and metabolic changes: Increased risk of diabetes and obesity.
- Cognitive changes: Some women report memory issues, though research is ongoing.
9. Can lifestyle changes really help?
Yes. Regular exercise strengthens bones and improves mood. A balanced diet rich in calcium and vitamin D supports bone health. Stress reduction techniques like yoga and meditation ease anxiety. Avoiding smoking and excessive alcohol reduces risks of early menopause and long-term complications.
10. Is menopause the same for every woman?
No. Experiences vary widely. Some women have few symptoms, while others struggle with severe hot flashes, mood swings, or sleep problems. Genetics, lifestyle, and health conditions all influence the severity and duration of symptoms.